






 When it comes to surgery, any good doctor will tell you that success is never guaranteed and there are always risks. But how does back surgery stack up compared to other treatments for back pain? The Mayo Clinic recommends caution before choosing back surgery. Their website warns, “Spine surgeons hold differing opinions about when to operate, what type of surgery to perform, and whether—for some spine conditions—surgery is warranted at all.” Always get a second opinion from a spine specialist.
When it comes to surgery, any good doctor will tell you that success is never guaranteed and there are always risks. But how does back surgery stack up compared to other treatments for back pain? The Mayo Clinic recommends caution before choosing back surgery. Their website warns, “Spine surgeons hold differing opinions about when to operate, what type of surgery to perform, and whether—for some spine conditions—surgery is warranted at all.” Always get a second opinion from a spine specialist.
One 2013 study in Washington State, published in the journal Spine, highlighted an interesting correlation between the number of back surgeries performed and the type of doctor first visited. The study found that of those injured workers who saw a surgeon first, 42.7% chose surgery (a relatively expensive and risky option) as a solution. Of those injured workers who first saw a chiropractor, the rate of surgeries dropped to 1.5%. In other words, those who visited a chiropractor first found that surgery was less likely to be necessary.
Research performed in Norway, with results published in the December 2012 edition of European Spine Journal, raised even more questions about the appropriateness or effectiveness of one common type of spine surgery. Two groups of patients were monitored over a 9-year period. Group membership was randomly assigned. One group received lumbar spinal fusion—a surgical procedure. The other group received exercises for coordination and endurance, plus mental training to reduce the amount of worry about further injury from going about their normal daily activities. In other words, this second group received physical and psychological training—no surgery.
In the surgery group, 68% were unable to work afterward, compared with only 42% in the non-surgery group. Of those who had surgery, 44% used medication for pain, while only 17% of those who didn’t have surgery used pain medication. Of the surgery group members, 17% were dissatisfied with the results they received. Of the non-surgery members, only 3% were unhappy with their outcomes. Those without surgery had a greater rate for return to work, less pain medication and greater satisfaction.
An earlier study found that of the 465,000 spinal fusions performed in America during 2011, as many as 50% had insufficient justification. Another study found physical therapy to be just as effective, but far less costly and risky than fusion surgery when attempting to solve the problem of degenerative disc disease.
There are of course situations where back surgery may be absolutely necessary. However, study after study has shown that other methods of treating back pain are far less expensive, less risky and frequently more effective. If you have been advised to have back surgery, it’s always good to get a second or even third opinion from different medical professionals to be sure you do not undergo a surgical procedure that may be best treated more conservatively.
 Whether they first see the phrase in print or hear it for the first time in a doctor’s office, “degenerative disc disease” is a term that many chronic back pain sufferers will encounter. It’s part of a brand new vocabulary that many patients learn as they try to understand their condition and navigate healthcare choices. But what does it really mean?
Whether they first see the phrase in print or hear it for the first time in a doctor’s office, “degenerative disc disease” is a term that many chronic back pain sufferers will encounter. It’s part of a brand new vocabulary that many patients learn as they try to understand their condition and navigate healthcare choices. But what does it really mean?
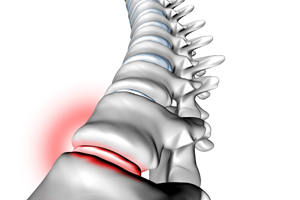
Degenerative disc disease is not actually a disease at all. Rather, it refers to normal changes in your spinal discs that tend to occur naturally as your body ages. Spinal discs are the soft “separators” between your vertebrae that cushion the individual bones and give your spine its flexibility. Healthy ones are thick and soft. Unhealthy ones are thinner and more brittle. Over the years, these discs may gradually become less effective as the amount of fluid inside is reduced or cumulative wear and tear damages the discs and raises the risk of bulging, rupture or disintegration. The truth is that by the time we reach middle age, most of us already have degenerating discs, whether we’re experiencing any pain or not. And even with our best imaging technology, it can be very difficult to tell whether this degeneration is actually the source of a patient’s problems.
So from a patient’s point of view, this bit of language-degenerative disc disease-can be both confusing and frustrating since it suggests a diagnosis but doesn’t usually come with a clear set of treatment options attached. In some ways, it may actually seem like a “catch-all diagnosis” or “un-diagnosis”.
Can I Benefit From Chiropractic Care if I Have Degenerative Disc Disease?
Sometimes patients who’ve been told they have degenerative disc disease wonder if chiropractic adjustments can still help them or if they’re safe. The answer to these questions depends on the patient’s individual circumstances, including whether the damaged discs are herniated or ruptured (bulging or broken) or have caused other conditions, such as osteoarthritis (a breakdown of the tissue that protects joints) or spinal stenosis (a narrowing of the channel within the spine that holds the spinal cord).
Chiropractic physicians are specially trained to diagnose the underlying causes of back pain and to recognize when specific types of treatment may be either ineffective or harmful in situations where patients have degenerative disc disease. Since they are often skilled in a wide range of conservative, non-surgical therapies, most chiropractors will recommend low-force, non-thrusting techniques in situations involving disc degeneration and related complications. They may also employ traditional spinal adjustments based upon the results of a careful evaluation of the patient.
Chiropractic care generally focuses on addressing back pain at its source as well as improving the spine’s stability and mobility. While there is no cure for degenerative disc disease, an effective treatment plan will usually combine manual therapies (such as manipulation or massage) with supervised exercise and/or nutritional programs and lifestyle changes designed to minimize its impact.